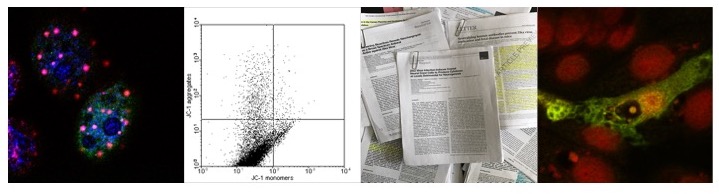
Research in animal models (chicken, mice, sheep, rats, goat, dogs and hamsters) indeed led to the identification of eight viruses to cause obesity in animals and research identified both human and animal Adenoviruses -specifically human Adenovirus 36 (Ad 36)- capable to infect adipocytes, resulting in the accumulation of triglycerides in adipocytes and changes in transcription factors involved in the differentiation of pre-adipocytes into (mature) adipocytes as well as in the modulation of the inflammatory response. Indeed, a higher percentage of obese (30%) than non-obese subjects (11%) tested seropositive for Adenovirus 36 antibodies.
Moreover, adenoviral induced obesity been implicated in increased risk of Influenza virus infection and morbidity during non-pandemic and pandemic Influenza seasons.
So how might pathogens like Adenovirus induce obesity and how might this contribute to increase risk of morbidity following infection with Influenza virus.
Inflammation and obesity
Experimentally this system can be induced by transfecting Poly (I:C), leading to the expression of leptin, resistin and adiponectin in mature adipocytes as well as the differentiation of pre-adipocytes into (mature) adipocytes. Blocking this system by using inhibitors specifically targeting IRF3 (BX795) or NF-κB (BAY11-7082) or using cells deficient in TLR-3 (TLR-3 -/-) showed that in particular RIG-1 or MDA5 are responsible for the inflammatory response since both are inducing the expression of pro-inflammatory cytokines. Notably, transfected Poly (I:C) inhibits the differ-entiation of pre-adipocytes to adipocytes and might thus contribute to increased insulin resistance. In addition, blocking this system might also be effect the expression of Interferon stimulated genes.
Poly (I:C) is considered to be mimetic of (specifically viral) dsRNA and does not occur in nature and stimulates TLR-3 in a wide variety of immune cells including dendritic cells and B-Lymphocytes.
What about the increased mortality due to obesity in patients in-fected with Influenza viruses? As outlined above, the activation of PPRs in pre-adipocytes downregulates the immune response and increases the expression of inflammatory cytokines. Indeed it is has been speculated that one reason of the increased morbidity in patients infected with A/H1N1/1918 was a “cytokine storm”. If however this is the case in the obese patients infected with current Influenza virus is open to speculation.
Finally, other pathogens might cause similar problems since the bacteria can induce an antibacterial response akin to the antiviral response.
Further reading:
van Ginneken V, Sitnyakowsky L, & Jeffery JE. (2009) "Infectobesity: viral infections (especially with human adenovirus-36: Ad-36) may be a cause of obesity. Medical hypotheses, 72(4), 383-8. PMID: 19138827
van Ginneken V, Sitnyakowsky L, & Jeffery JE. (2009) "Infectobesity: viral infections (especially with human adenovirus-36: Ad-36) may be a cause of obesity. Medical hypotheses, 72(4), 383-8. PMID: 19138827
Atkinson, Richard L. (2008-01--1) Could viruses contribute to the worldwide epidemic of obesity?. , 3(s1), 37-43. DOI: 10.1080/17477160801896754
Hur, Sun Jin. (2013-10--1) Effect of adenovirus and influenza virus infection on obesity. , 93(16), 531-535. DOI: 10.1016/j.lfs.2013.08.016
Cocoros, Noelle M. (2014-01--1) Obesity as a risk factor for severe influenza-like illness. , 8(1), 25-32. DOI: 10.1111/irv.12156 Yu, Lili. (2014-02--1) Pattern recognition receptor-initiated innate antiviral response in mouse adipose cells. , 92(2), 105-115. DOI: 10.1038/icb.2013.66
Genoni, Giulia. (2014-01--1) Obesity and infection: two sides of one coin. , 173(1), 25-32. DOI: 10.1007/s00431-013-2178-1