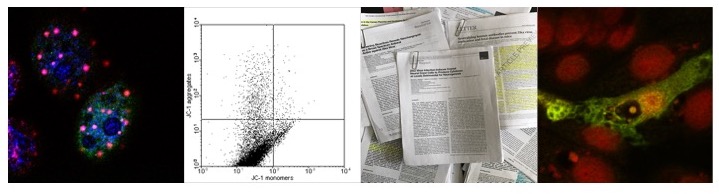
Under conditions of cell stress such as nutrient
deprivation or as a result of the accumulation of damaged organelles and
misfolded proteins a lysosomal pathway is induced which degrades proteins as
well organelles independent of the proteasomal pathway. The core machinery of
this pathway -termed autophagy from the Greek
auto-, "self" and phagein, "to eat” (literally
“selfeating”) - was discovered in genetic screens of yeast for genes required
for survival under nutrient starvation and since been shown to be conserved in
mammalian and plant cells alike, providing metabolic substrates in the absence
of external sources as well as contributing to cell survival by degrading
non-functional organelles. As discussed in previous posts, autophagy also
contributes to the degradation of viral proteins, the presentation of viral
antigens to the immune system via the MHC Class II system, as well as
contributing to the release of virions and the formation of replication
centers. In the context of viral infection therefore the induction of autophagy
can have both pro- as well as antiviral effects. Indeed, a number of viral
proteins such as the coronaviral nsp-6 or PLP2 proteins both induce the
formation of autophagosomes or autophagosome-like structures whilst preventing
the fusion of these structures with the lysosome whilst the genome of other
viruses encode for protein(s) which might prevent the fusion of autophagosomes
whilst not inducing the formation of autophagosomes. In addition to inducing
the degradation of viral proteins and/or viral RNA, the induction of autophagy
can also induce cell death, which in contrast to the induction apoptosis is
(primarily) independent of the induction of caspases and morphologically
different from apoptosis. In general, the induction of autophagy induced cell
death by cellular stress such as DNA damage, mitochondrial damage, or the
accumulation of misfolded proteins can be the result of defective
autophagy. Insufficient autophagy
characterized by a decrease of autophagy may induce both cell death and also
contribute to the immortalization of cells by failure of clearance of
micronuclei thus contributing to the accumulation reassembled chromosomes.
Excessive autophagy in contrast, induces lipid depletion of the ER and/or
nuclear membrane, and inducing a process termed autosis characterized by ER
fragmentation, which may be distinct from “classical” autophagy induced cell
death, the latter being induced by the release of Cathepsin-D and subsequent
activation of caspases.
 |
| Induction of different pathways due to dysregulated autophagy |
In contrast to autosis, which may or may not involve
the induction of ER stress response, the release of Cathepsin-D increases the
release of Cytochrome C and subsequent activates Caspase-3/-7 thus inducing the
depolarization of the mitochondrial membrane, linking defective autophagy to
Caspase-dependent apoptosis. Indeed, the overexpression of Cathepsin-D in human
malignant glioblastoma M059J cells induces autophagy and thus prevents
apoptosis. The connection between autophagy and apoptosis however is quite
complex, highlighted by results obtained from U87 human glioblastoma cells
treated with arsenic trioxide, in which the inhibition of autophagy using 3-MA
protects cells from arsenite toxicity whilst high concentrations of
Bafilomycin-A1 did not, indicating that the accumulation of mature lysosomes
induces apoptosis probably due to the release of Cathepsin-D, similar to
treatment of U87, LN229, LN308, U118 and U251 glioblastoma cell lines with
Chloroquine, and that low concentrations of Bafilomycin-A1 favors the downregulation
of Cathepsin-B and Cathepsin-L thus protecting cells from apoptosis.
In the case of Enterovirus-71 infected human
rhabdomyosarcoma (RD-A) cells, the increase of Cathepsin-D at 12 hrs p.i. has
been postulated to induce caspase-dependent apoptosis, whereas at earlier time
points the inhibition of the fusion of the autophagosome with the lysosome via
UVRAG and Bax prevents apoptosis; interestingly, the application of both
Z-VAD-FMK and Z-DEVD-FMK inhibitors not only prevents apoptosis but also promotes
autophagic flux as measured by the degradation of p62/SQSTM-1, indicating that
both processes are competing. In contrast to EV-71 infected RD-A cells,
Chloroquine treatment of the aforementioned glioblastoma cell lines however
induces caspase independent cell death, indicating that the outcome might be
cell line specific. It should be noted however that the involvement of caspases
in autophagy related cell death might be secondary and that caspase activation
might only be partial.
Generally, autosis is less well defined and might be
in fact a subtype of autophagy induced cell death. In cells undergoing autosis,
the ER is highly fragmented and focal ballooning of the perinuclear space can
be observed. Whilst being independent of caspase activation, autosis is induced
by excessive autophagy experimentally triggered by the expression of an
autophagy inducing peptide, Tat-Beclin, and dependent on the activity of the Na+/K+ ATPase.
So far, no viral protein or virus has been demonstrated to interfere with autosis
but it seems conceivable that the treatment of HIV, Chikungunya Virus, or West
Nile Virus infected cells with Tat-Beclin might trigger autosis.
 |
| Tat-Beclin might induce autosis in cells expressing HIV-Nef or degradation of Nef |
During the latent phase of the replication cycle, the EBV latent
membrane protein 1 (LMP-1) oncogene has been demonstrated to induce the
unfolded protein response (UPR)/ ER stress response pathway via the N terminal
six membrane spanning domain by activating all three branches of the UPR (PERK,
ATF6, and IRE-1) in a sequential manner. First, LMP-1 induces the expression
and activation of ATF4 via phosphorylation of eIF2α, thus inducing not only the
expression of LMP-1 but also inducing the expression of autophagy related genes,
preventing the induction of apoptosis due to prolonged induction of PERK.
Activation of IRE-1 promotes the accumulation of spliced XBP1, inducing the
formation of EDEMosomes via increasing the expression of EDEM-1 and EDEM-2 as
well as the activating Beclin-1 by JNK mediated phosphorylation of Bcl-2 whilst
inhibiting autophagy via CHOP. Cleavage of ATF6 generates ATF6α, inducing the
ERAD pathway and activating CHOP. Translocation of ATF6α from the ER/Golgi into
the nucleus increases the expression of EBV genes, thus promoting expression of
viral genes. An increased level of phosphorylated eIF2α however inhibits
general translation, lowering LMP-1 levels, allowing the cycle to begin anew.
High levels of autophagy induced via the UPR, thus promoting cell
survival, also degrade LMP-1. Indeed, transfection of EBV infected
B-lymphocytes with siBeclin-1 not only inhibits LMP-1 induced autophagy but
also increases LMP-1 levels and induces apoptosis. LMP-1 induced autophagy
therefore has a pro-survival rather than an pro-apoptotic effect, at least in
the context of viral infection. In addition to autophagy induced as a result of
ER stress, LMP-1 might induce the formation of autophagosomes via induction of
PI3K.
 |
| EBV LMP-1 |
 |
| EBV LMP-2A |
The expression of another EBV latent membrane protein, LMP-2A, also
induces autophagy and prevents apoptosis/anoikis in human nonmalignant breast
epithelial MCF10A cells. In this case, blocking the formation of autophagosomes
with 3-MA or the degradation of the autolysosome with Chloroquine not only
prevents autophagy but also induces the cleavage of Caspase-3. Conversely, the
expression of LMP-2 in the absence of inhibitors promotes the formation of
autophagosomes in a Atg5 and Atg7 dependent manner probably involving the
K11-ubiquitiylation of Beclin-1 by NEDD4 E3 ubiquitin ligases such as Itch or
RNF5 as well as cleavage of ATG4B cysteine protease and subsequent lipidation
of LC3-I (converting LC3-I to LC3-II)
via the PY domain. LMP-2A therefore might facilitate the lipidation of
LC3-I -and thus the formation of the mature autophagosome- by ATG4B mediated
cleavage of LC3-I. In addition, LMP-2A forms a complex with ATG5 and ATG12,
implying that LMP-2A induces the formation of the phagophore by sequestering Beclin-1,
leading to the recruitment of Vps34, UVRAG, AMBRA1, ATG14L, p150 and/or Bif-1
independent of ULK-1 as well as promoting the conversion of LC3-I to LC3-II.
 |
| Regulation of autophagy in cells expressing both LMP-1 and LMP2A: model |
In the context of viral infection both LMP-1 and LMP-2A
co-localize to lipid rafts, indicating that lipid rafts are the membrane source
for the autophagic vesicles induced by both proteins, similar to HTLV-1 Tax.
Since the expression of LMP-1 induces the ER stress response, it might be
possible that LMP-2A increases the clearance of LMP-1 by enhancing LMP-1
induced autophagy. It remains to be seen if the combined
expression of both LMP-1 and LMP-2A in the absence of other viral proteins such
as EBNA-1 induces autophagic cell death or autosis due to lipid depletion. Also
it remains to be seen if the induction of autophagy by LMP-1 and/or LMP-2A
interferes with immune sensing pathways, including STING mediated signaling by
clearing mitochondria bound to the ER via MAM. Moreover, the induction of
autophagy by EBV has been demonstrated to decrease viral replication and
autophagic flux is inhibited in EBV infected cells entering the lytic cycle.
Since both LMP-1 and LMP-2A are expressed during latency, LMP-1/LMP-2A induced
autophagy might be essential to maintain latency. If the experimental inhibition
of LMP-1 and/or LMP-2A induced autophagy is however sufficient to abolish
latency remains to be seen.
Further reading
Xu T, Nicolson S, Denton D, & Kumar S (2015). Distinct requirements of Autophagy-related genes in programmed cell death. Cell death and differentiation PMID: 25882046
Geng Y, Kohli L, Klocke BJ, & Roth KA (2010). Chloroquine-induced autophagic vacuole accumulation and cell death in glioma cells is p53 independent. Neuro-oncology, 12 (5), 473-81 PMID: 20406898
Pucer A, Castino R, Mirković B, Falnoga I, Slejkovec Z, Isidoro C, & Lah TT (2010). Differential role of cathepsins B and L in autophagy-associated cell death induced by arsenic trioxide in U87 human glioblastoma cells. Biological chemistry, 391 (5), 519-31 PMID: 20302512
Xi X, Zhang X, Wang B, Wang T, Wang J, Huang H, Wang J, Jin Q, & Zhao Z (2013). The interplays between autophagy and apoptosis induced by enterovirus 71. PloS one, 8 (2) PMID: 23437282
Bhoopathi P, Chetty C, Gujrati M, Dinh DH, Rao JS, & Lakka S (2010). Cathepsin B facilitates autophagy-mediated apoptosis in SPARC overexpressed primitive neuroectodermal tumor cells. Cell death and differentiation, 17 (10), 1529-39 PMID: 20339379
Hah YS, Noh HS, Ha JH, Ahn JS, Hahm JR, Cho HY, & Kim DR (2012). Cathepsin D inhibits oxidative stress-induced cell death via activation of autophagy in cancer cells. Cancer letters, 323 (2), 208-14 PMID: 22542809
Liu Y, & Levine B (2015). Autosis and autophagic cell death: the dark side of autophagy. Cell death and differentiation, 22 (3), 367-76 PMID: 25257169
Muñoz-Pinedo, C., & Martin, S. (2014). Autosis: a new addition to the cell death tower of babel Cell Death and Disease, 5 (7) DOI: 10.1038/cddis.2014.246
Liu Y, Shoji-Kawata S, Sumpter RM Jr, Wei Y, Ginet V, Zhang L, Posner B, Tran KA, Green DR, Xavier RJ, Shaw SY, Clarke PG, Puyal J, & Levine B (2013). Autosis is a Na+,K+-ATPase-regulated form of cell death triggered by autophagy-inducing peptides, starvation, and hypoxia-ischemia. Proceedings of the National Academy of Sciences of the United States of America, 110 (51), 20364-71 PMID: 24277826
Young, L., & Rickinson, A. (2004). Epstein–Barr virus: 40 years on Nature Reviews Cancer, 4 (10), 757-768 DOI: 10.1038/nrc1452
Busson P, McCoy R, Sadler R, Gilligan K, Tursz T, & Raab-Traub N (1992). Consistent transcription of the Epstein-Barr virus LMP2 gene in nasopharyngeal carcinoma. Journal of virology, 66 (5), 3257-62 PMID: 1313931
Fotheringham JA, & Raab-Traub N (2015). Epstein Barr-Virus Latent Membrane Protein 2 Induces Autophagy to Prevent Cell Death. Journal of virology PMID: 25878108
Longnecker R, & Kieff E (1990). A second Epstein-Barr virus membrane protein (LMP2) is expressed in latent infection and colocalizes with LMP1. Journal of virology, 64 (5), 2319-26 PMID: 2157888
Granato M, Santarelli R, Farina A, Gonnella R, Lotti LV, Faggioni A, & Cirone M (2014). Epstein-barr virus blocks the autophagic flux and appropriates the autophagic machinery to enhance viral replication. Journal of virology, 88 (21), 12715-26 PMID: 25142602
Li Y, Zhang L, Zhou J, Luo S, Huang R, Zhao C, & Diao A (2015). Nedd4 E3 ubiquitin ligase promotes cell proliferation and autophagy. Cell proliferation PMID: 25809873
Kuang E, Qi J, & Ronai Z (2013). Emerging roles of E3 ubiquitin ligases in autophagy. Trends in biochemical sciences, 38 (9), 453-60 PMID: 23870665
Abrahamsen H, Stenmark H, & Platta HW (2012). Ubiquitination and phosphorylation of Beclin 1 and its binding partners: Tuning class III phosphatidylinositol 3-kinase activity and tumor suppression. FEBS letters, 586 (11), 1584-91 PMID: 22673570
Xia P, Wang S, Du Y, Zhao Z, Shi L, Sun L, Huang G, Ye B, Li C, Dai Z, Hou N, Cheng X, Sun Q, Li L, Yang X, & Fan Z (2013). WASH inhibits autophagy through suppression of Beclin 1 ubiquitination. The EMBO journal, 32 (20), 2685-96 PMID: 23974797
Naon D, & Scorrano L (2014). At the right distance: ER-mitochondria juxtaposition in cell life and death. Biochimica et biophysica acta, 1843 (10), 2184-94 PMID: 24875902
Frappier L (2012). Contributions of Epstein-Barr nuclear antigen 1 (EBNA1) to cell immortalization and survival. Viruses, 4 (9), 1537-47 PMID: 23170171