Arboviruses such as Dengue Virus (DENV), Chikungunya
Virus (CHIKV) or Zika Virus (ZIKV) are arthropod borne viruses that are
transmitted to humans via a relatively small number of mosquito species, in
particular Aedes spp. and Culex spp., and only rarely does human-to-human
transmission occur. Humans and other vertebrate animals may serve as a
secondary host and in the absence of human-to-human transmission as a reservoir
host. Indeed, uninfected (female) mosquitoes only become infected following a
blood meal from an infected vertebrae. Following viral infection, the viral
particle then needs to enter epithelial cells of the midgut where viral
replication takes place, followed by the egress of viral particles into
hemocoel and subsequent spread into the salivary glands, thus allowing the
infection of humans and/or animals via an insect bite. Within the insect, both
the salivary gland and the midgut are therefore natural barriers to viral
replication.
Similar to the human gut, the insect gut contains an
abundant bacterial flora that may inhibit or promote viral entry as well as
viral replication, including obligate intracellular symbionts that may prevent
viral replication. In the case of Aedes Agypti experimentally infected
with DENV-serotype 2 (DENV-2), treatment with antibiotics reduces viral titres,
and co-infection of midgut epithelial cells of Ae. aegypti larvae and
adults with DENV-2 or CHIKV and Serrata odoroferia (a gram-negative,
anaerobic, bacteria of the Enterobacteriaceae) increases susceptibility
of Ae.aegypti to DENV-2 and CHIKV in the absence of increased viral
replication suggesting that bacteria can at least facilitate viral entry. In
the case of midgut epithelial cells co-infected with CHIKV and S.odoroferia,
CHIKV has been shown to interact with two mitochondrial proteins, namely Hsp60
and Porin.
Furthermore,
the co-infection of Ae. aqypti but not Ae. notoscriptus with both DENV and Wolbachia pipientis decreases
viral replication, although the mechanism is not known. It has been speculated
however that the infection of cells with Wolbachia induces the immune response,
which not only targets bacteria but also DENV and -in Ae.albopictus-
derived C6/36 cells also inhibits the replication of DENV and CHIKV as shown by
decreased levels of viral RNA and viral titres.
CHIKV
and Wolbachia Hsp60 protein
 |
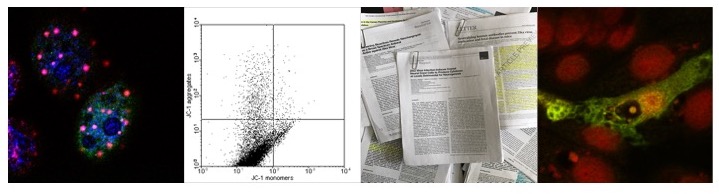
| Figure: CHIKV and the ER stress response |
Interestingly, the treatment of PBMCs but not
lymphocytes derived from both asymptomatic endemic normal and chronic patients
with purified recombinant Wolbachia
Hsp60 (rWMhsp60) induces caspase-dependent apoptosis, which can be inhibited by
autophagy. Apoptosis is induced by the activation of TLR-4 receptors at the
cell surface and inducing the formation of reactive oxygen species (ROS) in
mitochondria. As a result, mitochondrial membrane potential depolarizes,
cytochrome C is released and subsequently downstream caspases (caspase-3 and
-9) are activated, inducing caspase dependent cell death. In addition, recent research indicates that ROS also induces a
variant of autophagy termed NETosis (Neutrophil
extracellular traps), suggesting that Wolbachia
and/or rWMHsp60 might induce cell death in the absence of classical apoptotic
markers such as exposure of Phosphatidylserine. Activation of TLR-4 however may
also induce autophagy via TRIF/MyD88 mediated cleavage of the Bcl-2/Beclin-1 complex
and thus contributes to the formation of the phagosomes. Subsequently,
bacterial induced autophagy may induce the cellular antibacterial response as
well as promoting the presentation of antigens via the MHC Class II complex.
 |
| Figure: Binding of rWMhsp60 to TLR-4 stimulates NETosis and/or caspase dependent apoptosis |
 |
| Figure: WMHsp60 might activate TLR-4 induced formation of ROS and thus promotes the degradation viral RC |
Treatment of cells derived from endemic normal but not
chronic patients with Rapamycin and purified rWMhsp60 however induces not only
the formation of autophagosomes but also prevents apoptosis; if autophagic flux
is inhibited has not been demonstrated, although the results suggest that this
is the case since TLR-4 localises inside LC3 positive vesicles. In any case,
these results suggest that C3/36 cells infected with CHIKV may undergo
apoptosis in the presence of Wolbachia or at least if expressing
WMhsp60. Alternatively, Wolbachia derived Hsp60 might sequester CHIKV
viral particles and/or CHIKV viral proteins, thus inhibiting release of the
viral genome, viral assembly, and/or viral egress. Whilst this has not been
investigated yet, it is known that in cells derived from the midgut epithelium
and infected with both CHIKV and Wolbachia, CHIKV binds to Hsp60. Given
that in cells treated rWMhsp60 apoptosis is induced by depolarization of the
mitochondrial membrane, the induction of autophagy by rapamycin might induce
mitophagy; consequently CHIKV (bound to mitochondrial Hsp60) might be degraded
by mitophagy. In addition, the co-infection with CHIKV may promote the
presentation of both viral and bacterial antigens via the MHC Class II complex
and thus promote the induction of the immune response.
It should be noted however that Hsp60 is also located
at the cell surface and rWMhsp60 has been reported to interact with cell
surface TLR-4, leading to the activation of a pro-apoptotic cell signaling
pathway including the induction of oxidative stress signaling and the
activation of caspase-3. The induction of autophagy by Rapamycin relocalises
TLR-4 to late endosomes thus preventing the activation of the pathways.
Analogous to Rapamycin treatment, the induction of the ER stress response by
CHIKV might relocalise TLR-4 in rWMHsp60 treated mosquito cells as well, thus
inhibiting antiviral as well as antibacterial signaling pathways.
The problem is that any effect on the autophagic flux
has not been evaluated and consequently any effect on the stability on the
viral RC is only hypothetic. If autophagic flux however increases in Rapamycin
treated and Wolbachia infected cells, then the co-infection with CHIKV
might induce the degradation of not only TLR-4 (and thus protect cells from Wolbachia induced apoptosis) but also of
the viral RC (and thus decrease viral replication) particularly at early stages
of viral replication during formation of the RC.
In conclusion, Wolbachia might either sequester
viral particles and/or viral proteins via WMhsp60 or alternatively CHIKV
induced formation of autophagosomes might facilitate the degradation of TLR-4
and viral RC, thus not only preventing apoptosis (and senescence) but also
leading to reduced viral replication. Additionally, inducing the degradation of
viral RCs and/or TLR-4 following the infection of Wolbachia containing cells
might also degrade Wolbachia itself since the induction of autophagy has also
been shown to degrade Wolbachia in C3/36 and PC35 cells.
DENV and Wolbachia: inhibition of viral entry
v. protection of WMHsp60 induced apoptosis
In the case of DENV, the viral NS1 protein has been
reported to localize to vesicular structures containing the viral NS5, NS3,
NS2A, NS2B, NS4A and NS1 proteins as well as dsRNA and the viral RNA dependent
RNA Polymerase (RdRP) in infected Vero and C6/36 cells. In subsequent studies,
it was shown that the formation of viral RC -similar to other positive strand
viruses such as Poliovirus and Coronaviruses- is dependent on autophagy as
evidenced by decreased viral replication in autophagy deficient MEF cells,
knockdown of autophagy related genes, or treatment with 3-Methyladenine (3-MA)
of DENV-2 or DENV-3 infected human Pre-Basophils/Mast KU812, Huh7 and HepG2
cells as well as increased viral replication in DENV-3 infected HepG2 cells
treated with Rapamycin. DENV RC however do not represent classical
autophagosomes but rather invaginations of ER cisternae that may mature into
amphisomes as a result of the fusion of endosomes with autophagosomes as
indicated by the co-localization of dsRNA with mannose-6-phosphate receptor
(MPR) as well as LC3. In addition, DENV inhibits Torin-1 induced, starvation
induced and basal autophagic flux in Huh7 cells as evidenced by the use of a
mCherry-LC3 reporter plasmid whilst inducing the proteasomal degradation of p62/SQSTM-1,
suggesting that the formation of viral RC indeed might be not entirely
dependent on autophagy related proteins. The induction of autophagy by DENV
however is required for the degradation of lipid droplets and the release of
lipids thus stimulating lipid metabolism via selective autophagy.
 |
| Figure: DENV induction of lipophagy - connection to mitophay? |
Similar to other viruses, DENV therefore has been
postulated to induce the formation of autophagosome or autophagosome-like
structures early in the replication cycle whilst inhibiting autophagic flux
later in the replication cycle.
In the case of mosquito cells, C3/36 cells infected
with DENV support the findings obtained from mammalian cells is so far as the
viral RC are in close proximity to the ER and coated with ribosomes (similar to
the co-localization of dsRNA with L28 in DENV-2 infected HepG2 cells) and similar to mammalian cells, cellular
fatty acid synthase is redistributed to the viral RC (by the viral NS3 protein
and dependent on Rab18).
The degradation of lipid droplets by DENV induced
autophagy might therefore be conserved in both mammalian and mosquito cells. In
the case of mosquito cells infected with both Wolbachia and DENV
however, DENV might prevent cells from WMhsp60 induced apoptosis and senescence
by either sequestering TLR-4 in amphisomes and/or degradation of TLR-4 at least
early in infection whereas later in infection due to the inhibition of
autophagic flux TLR-4 might accumulate in late endosomes or amphisomes.
However, this might only apply if the infection of
cells with DENV occurs prior the infection with Wolbachia since Wolbachia
has been reported to prevent the entry of DENV and other Flavivirus' into cells
by sequestering cholesterol. In contrast, Serratia odorifera
might increase viral entry by increasing prohibitin on the cell surface.
Mitochondria localized prohibitin has also been shown to inhibit mitophagy, but
in the absence of data it is not possible to discern if Serratia odorifera
induces merely the redistribution of either HSP60 and/or Prohibitin or
alternatively promotes the redistribution of mitochondria to sites of viral
replication. The pore forming ShlA toxin from Serratia marcesens has
been shown to induce autophagy in CHO cells, a potential homologoue in Serratia
odorifera might increase DENV replication by facilitating the fusion of
lipid droplets with autophagosomes and lysosomes.
Lipophagy:
autophagy of lipid droplets
Autophagy has been shown to regulate the metabolism of
lipid droplets that are storage areas of triglycerides (TG) and cholesterol
both in the absence and presence of viral replication. The induction of
autophagy correlates with the decrease of triglyceride levels since the fusion
of lipid droplets (LD) with autophagosomes and subsequent lysosomal fusion induces
the release of free fatty acids in a process commonly referred to as lipophagy
which requires both lipases and the small Rab7GTPase. Free fatty acids released
by lipophagy generate ATP by mitochondrial β-oxidation and thus contribute to the maintenance of the cellular energy homeostasis. In the
context of viral replication, Brome Mosaic Virus replication is dependent on
specific localised lipid compositions whereas West Nile Virus induces the
synthesis and redistribution of cholesterol to sites of viral replication. In
the case of Hepatitis C Virus (HCV) -arguably the most prominent virus that
utilises lipid droplets for viral replication- assembly of viral particles
takes place at lipid droplets and the release of viral particles is dependent
on the very low-density lipid secretion pathway.
Inf DENV-2 infected Huh 7.5 cells, the induction of
autophagy not only protects cells from apoptosis induced by the UPR pathway but
also decreases TG levels and LD area by approx. 35% (leading to a reduction of
approx. 70% of the LD volume) as measured by oil red staining and EM
respectively at 48 hrs p.i. .Treatment of infected cells with either 3-MA or
transfection with siRNA targeting Beclin-1 or ATG12 prior infection results in
a marked increase in LD compared to mock treated cells, indicating that indeed
not only the induction of autophagy is necessary for DENV-2 induced lipophagy.
Accordingly, lipophagy should be inhibited at later stages of the replication
cycle. Rather than inducing the formation of autophagosomes however, DENV-2
might rather promote the fusion of autophagosomes with LD as indicated by
results showing that the number of lysosomes is not altered in DENV-2 infected
Huh 7.5 cells but that the number of structures positive for both Bodipy 493/503
and Lysotracker increases. Using a novel
inhibitor, SAR-405, which targets the Vps34 kinase should clarify if DENV-2
does induce the formation of mitophagosomes akin to HCV or alternatively
promotes the fusion of existing autophagosomes independent of de novo
formed mitophagosomes. So far however DENV NS4A has not been shown to exhibit
mitochondrial localisation in infected Huh 7 cells. The free fatty acids
generated by the degradation of TG however are not utilised to generate ATP but
also required for the formation of viral particles; free fatty acids are
recruited to viral RC via an interaction between the viral DENV NS3 protein
localised at the ER and free fatty acids in a Rab18GTPase dependent manner. In
addition to mitophagy, lipid droplets may also be degraded by autophagy.
 |
| Figure: DENV and ZIKV induce autophagy and/or mitophagy and lipophagy |
Recent evidence however suggests that in Aag-2 cells derived from Aedes Aqypti, both the infection with bacteria and with Sindbis Virus (SINV) or DENV increases the number of LD, suggesting that the induction of LD synthesis induces the antiviral and antibacterial response. It should be noted however that the authors did not evaluate lipophagy and/or the co-localisation of LD with LC3 in these cells.
Similar to Vero cells transfected with the
Polyomavirus BK Angnoprotein or Polyomavirus BK infected cells, LD in DENV-2
infected cells are localised in close proximity to the ER, which is in
accordance with the site of viral replication, but similar to DENV, an
accumulation of mitoplysophagsomes has not been demonstrated for Polyomavirus.
.
In the case of co-infection of cells with DENV-2 and Serratia
odorifera, mitochondria might
relocated to the site of viral
replication and thus increase the availability of ATP provided if the bacterial
HSP60 and/or Prohibitin localises to the mitochondria of the host cell and
interacts with viral proteins localised at the ER. If these mitochondria are
susceptible to depolarisation and undergo mitophagy remains also to be seen.
Finally in my opinion, DENV might increase replication
of ZIKV by increasing the turnover of LD, thus providing a favourable
environment for ZIKV replication.\
In summary, both Wolbachia and Serratia odorifera might play an important role in regulating the replication of CHIKV, DENV, and potentially ZIKV in mosquito cells both by decreasing and increasing viral titres. Further research is however need to establish the nature of these interactions.

In summary, both Wolbachia and Serratia odorifera might play an important role in regulating the replication of CHIKV, DENV, and potentially ZIKV in mosquito cells both by decreasing and increasing viral titres. Further research is however need to establish the nature of these interactions.
Further reading
Clem RJ (2016). Arboviruses and apoptosis: the role of cell death in determining vector competence. The Journal of general virology PMID: 26872460
Franz AW, Kantor AM, Passarelli AL, & Clem RJ (2015). Tissue Barriers to Arbovirus Infection in Mosquitoes. Viruses, 7 (7), 3741-67 PMID: 26184281
Hegde S, Rasgon JL, & Hughes GL (2015). The microbiome modulates arbovirus transmission in mosquitoes. Current opinion in virology, 15, 97-102 PMID: 26363996
Jupatanakul N, Sim S, & Dimopoulos G (2014). The insect microbiome modulates vector competence for arboviruses. Viruses, 6 (11), 4294-313 PMID: 25393895
Vaidyanathan R, & Scott TW (2006). Apoptosis in mosquito midgut epithelia associated with West Nile virus infection. Apoptosis : an international journal on programmed cell death, 11 (9), 1643-51 PMID: 16820968
Weaver SC, Scott TW, Lorenz LH, Lerdthusnee K, & Romoser WS (1988). Togavirus-associated pathologic changes in the midgut of a natural mosquito vector. Journal of virology, 62 (6), 2083-90 PMID: 2896802
Coffey LL, Failloux AB, & Weaver SC (2014). Chikungunya virus-vector interactions. Viruses, 6 (11), 4628-63 PMID: 25421891
Apte-Deshpande AD, Paingankar MS, Gokhale MD, & Deobagkar DN (2014). Serratia odorifera mediated enhancement in susceptibility of Aedes aegypti for chikungunya virus. The Indian journal of medical research, 139 (5), 762-8 PMID: 25027087
Kamalakannan V, Shiny A, Babu S, & Narayanan RB (2015). Autophagy protects monocytes from Wolbachia heat shock protein 60-induced apoptosis and senescence. PLoS neglected tropical diseases, 9 (4) PMID: 25849993
Xu Y, Jagannath C, Liu XD, Sharafkhaneh A, Kolodziejska KE, & Eissa NT (2007). Toll-like receptor 4 is a sensor for autophagy associated with innate immunity. Immunity, 27 (1), 135-44 PMID: 17658277
Delgado MA, & Deretic V (2009). Toll-like receptors in control of immunological autophagy. Cell death and differentiation, 16 (7), 976-83 PMID: 19444282
Remijsen Q, Kuijpers TW, Wirawan E, Lippens S, Vandenabeele P, & Vanden Berghe T (2011). Dying for a cause: NETosis, mechanisms behind an antimicrobial cell death modality. Cell death and differentiation, 18 (4), 581-8 PMID: 21293492
Stoiber W, Obermayer A, Steinbacher P, & Krautgartner WD (2015). The Role of Reactive Oxygen Species (ROS) in the Formation of Extracellular Traps (ETs) in Humans. Biomolecules, 5 (2), 702-23 PMID: 25946076
Miller, S., Kastner, S., Krijnse-Locker, J., Buhler, S., & Bartenschlager, R. (2007). The Non-structural Protein 4A of Dengue Virus Is an Integral Membrane Protein Inducing Membrane Alterations in a 2K-regulated Manner Journal of Biological Chemistry, 282 (12), 8873-8882 DOI: 10.1074/jbc.M609919200
Ruggieri V, Mazzoccoli C, Pazienza V, Andriulli A, Capitanio N, & Piccoli C (2014). Hepatitis C virus, mitochondria and auto/mitophagy: exploiting a host defense mechanism. World journal of gastroenterology, 20 (10), 2624-33 PMID: 24627598
Unterstab G, Gosert R, Leuenberger D, Lorentz P, Rinaldo CH, & Hirsch HH (2010). The polyomavirus BK agnoprotein co-localizes with lipid droplets. Virology, 399 (2), 322-31 PMID: 20138326
Schroeder B, Schulze RJ, Weller SG, Sletten AC, Casey CA, & McNiven MA (2015). The small GTPase Rab7 as a central regulator of hepatocellular lipophagy. Hepatology (Baltimore, Md.), 61 (6), 1896-907 PMID: 25565581
Goeritzer M, Vujic N, Schlager S, Chandak PG, Korbelius M, Gottschalk B, Leopold C, Obrowsky S, Rainer S, Doddapattar P, Aflaki E, Wegscheider M, Sachdev V, Graier WF, Kolb D, Radovic B, & Kratky D (2015). Active autophagy but not lipophagy in macrophages with defective lipolysis. Biochimica et biophysica acta, 1851 (10), 1304-16 PMID: 26143381
Liu K, & Czaja MJ (2013). Regulation of lipid stores and metabolism by lipophagy. Cell death and differentiation, 20 (1), 3-11 PMID: 22595754
Heaton NS, & Randall G (2010). Dengue virus-induced autophagy regulates lipid metabolism. Cell host & microbe, 8 (5), 422-32 PMID: 21075353
Mackenzie JM, Jones MK, & Young PR (1996). Immunolocalization of the dengue virus nonstructural glycoprotein NS1 suggests a role in viral RNA replication. Virology, 220 (1), 232-40 PMID: 8659120
Richards AL, & Jackson WT (2013). How positive-strand RNA viruses benefit from autophagosome maturation. Journal of virology, 87 (18), 9966-72 PMID: 23760248
Fang YT, Wan SW, Lu YT, Yao JH, Lin CF, Hsu LJ, Brown MG, Marshall JS, Anderson R, & Lin YS (2014). Autophagy facilitates antibody-enhanced dengue virus infection in human pre-basophil/mast cells. PloS one, 9 (10) PMID: 25329914
Metz P, Chiramel A, Chatel-Chaix L, Alvisi G, Bankhead P, Mora-Rodriguez R, Long G, Hamacher-Brady A, Brady NR, & Bartenschlager R (2015). Dengue Virus Inhibition of Autophagic Flux and Dependency of Viral Replication on Proteasomal Degradation of the Autophagy Receptor p62. Journal of virology, 89 (15), 8026-41 PMID: 26018155
Ronan B, Flamand O, Vescovi L, Dureuil C, Durand L, Fassy F, Bachelot MF, Lamberton A, Mathieu M, Bertrand T, Marquette JP, El-Ahmad Y, Filoche-Romme B, Schio L, Garcia-Echeverria C, Goulaouic H, & Pasquier B (2014). A highly potent and selective Vps34 inhibitor alters vesicle trafficking and autophagy. Nature chemical biology, 10 (12), 1013-9 PMID: 25326666
Di Venanzio G, Stepanenko TM, & García Véscovi E (2014). Serratia marcescens ShlA pore-forming toxin is responsible for early induction of autophagy in host cells and is transcriptionally regulated by RcsB. Infection and immunity, 82 (9), 3542-54 PMID: 24914224
Kathiria AS, Butcher LD, Feagins LA, Souza RF, Boland CR, & Theiss AL (2012). Prohibitin 1 modulates mitochondrial stress-related autophagy in human colonic epithelial cells. PloS one, 7 (2) PMID: 22363587
Kuadkitkan A, Wikan N, Fongsaran C, & Smith DR (2010). Identification and characterization of prohibitin as a receptor protein mediating DENV-2 entry into insect cells. Virology, 406 (1), 149-61 PMID: 20674955
Le Clec'h W, Braquart-Varnier C, Raimond M, Ferdy JB, Bouchon D, & Sicard M (2012). High virulence of Wolbachia after host switching: when autophagy hurts. PLoS pathogens, 8 (8) PMID: 22876183
Rothwell C, Lebreton A, Young Ng C, Lim JY, Liu W, Vasudevan S, Labow M, Gu F, & Gaither LA (2009). Cholesterol biosynthesis modulation regulates dengue viral replication. Virology, 389 (1-2), 8-19 PMID: 19419745
Skelton E, Rancès E, Frentiu FD, Kusmintarsih ES, Iturbe-Ormaetxe I, Caragata EP, Woolfit M, & O'Neill SL (2015). A Native Wolbachia Endosymbiont Does Not Limit Dengue Virus Infection in the Mosquito Aedes notoscriptus (Diptera: Culicidae). Journal of medical entomology PMID: 26721865
Stevanovic AL, Arnold PA, & Johnson KN (2015). Wolbachia-mediated antiviral protection in Drosophila larvae and adults following oral infection. Applied and environmental microbiology, 81 (23), 8215-23 PMID: 26407882
Tang WC, Lin RJ, Liao CL, & Lin YL (2014). Rab18 facilitates dengue virus infection by targeting fatty acid synthase to sites of viral replication. Journal of virology, 88 (12), 6793-804 PMID: 24696471
Heaton NS, Perera R, Berger KL, Khadka S, Lacount DJ, Kuhn RJ, & Randall G (2010). Dengue virus nonstructural protein 3 redistributes fatty acid synthase to sites of viral replication and increases cellular fatty acid synthesis. Proceedings of the National Academy of Sciences of the United States of America, 107 (40), 17345-50 PMID: 20855599
Junjhon J, Pennington JG, Edwards TJ, Perera R, Lanman J, & Kuhn RJ (2014). Ultrastructural characterization and three-dimensional architecture of replication sites in dengue virus-infected mosquito cells. Journal of virology, 88 (9), 4687-97 PMID: 24522909
Paul, D., & Bartenschlager, R. (2015). Flaviviridae Replication Organelles: Oh, What a Tangled Web We Weave Annual Review of Virology, 2 (1), 289-310 DOI: 10.1146/annurev-virology-100114-055007
Perera R, Riley C, Isaac G, Hopf-Jannasch AS, Moore RJ, Weitz KW, Pasa-Tolic L, Metz TO, Adamec J, & Kuhn RJ (2012). Dengue virus infection perturbs lipid homeostasis in infected mosquito cells. PLoS pathogens, 8 (3) PMID: 22457619
Panyasrivanit M, Khakpoor A, Wikan N, & Smith DR (2009). Co-localization of constituents of the dengue virus translation and replication machinery with amphisomes. The Journal of general virology, 90 (Pt 2), 448-56 PMID: 19141455
Huang J, Li Y, Qi Y, Zhang Y, Zhang L, Wang Z, Zhang X, & Gui L (2014). Coordinated regulation of autophagy and apoptosis determines endothelial cell fate during Dengue virus type 2 infection. Molecular and cellular biochemistry, 397 (1-2), 157-65 PMID: 25138703
Lee, Y., Hu, H., Kuo, S., Lei, H., Lin, Y., Yeh, T., Liu, C., & Liu, H. (2013). Dengue virus infection induces autophagy: an in vivo study Journal of Biomedical Science, 20 (1) DOI: 10.1186/1423-0127-20-65
Ana Beatriz Ferreira Barletta, Liliane Rosa Alves, Maria Clara L. Nascimento Silva, Shuzhen Sim, George Dimopoulos, Sally Liechocki, Clarissa M. Maya-Monteiro & Marcos H. Ferreira Sorgine
Emerging role of lipid droplets in Aedes aegypti immune response against bacteria and Dengue virus
Scientific Reports 6:19928
Emerging role of lipid droplets in Aedes aegypti immune response against bacteria and Dengue virus
Scientific Reports 6:19928