Both cellular and viral proteins translocate into the
Endoplasmic Reticulum to be post-translationally modified by ER resident
glycosylases and folded by ER president chaperones prior being transported to
other cellular organelles and/or being exported to the plasma membrane for
release. The accumulation of proteins of misfolded or unfolded proteins within
the ER results in the induction of the ER stress response -also known as
Unfolded Protein Response (UPR)- as described elsewhere. In general, this process
involves the increased expression of genes encoding for chaperones as well as
the reduction of both transcription and translation as well as the induction of
autophagy; prolonged ER stress however can lead to the induction of apoptosis
via intrinsic pathways involving the depolarisation of the mitochondrial
membrane. UPR is initiated by the
dissociation of Ca2+ dissociated heavy chain binding protein
(BiP)/Glucose regulated Protein 78 (GRP78) from dsRNA RNA dependent protein
kinase (PERK), thus allowing PERK to phosphorylate the alpha subunit of the
eukaryotic translation factor-2 (eIF2α), which in turn inhibits translation.
Phosphorylated eIF2α also selectively increases the translation of Activating
Transcription Factor- 4 (ATF4). As outlined before, ATF4 increases the
expression of CHOP/GADD153, thus in turn not only upregulates apoptosis but
also autophagy via upregulation of Beclin-1.
CHOP expression is however also induced by the two other branches of the
UPR, namely the IRE1- and ATF6α.
Chikungunya virus (CHIKV) is the causative agent of an arthropod (mosquito) transmitted disease which is characterised by a high fever, rash, joint pain, and arthritis which was reported in 1952 in Tanzania but has spread since to Europe, Asia, Oceania and more recently to America, including the Caribbean and North America.
 |
| The ER stress response: three branches which are intersected |
Chikungunya virus (CHIKV) is the causative agent of an arthropod (mosquito) transmitted disease which is characterised by a high fever, rash, joint pain, and arthritis which was reported in 1952 in Tanzania but has spread since to Europe, Asia, Oceania and more recently to America, including the Caribbean and North America.
 |
| Chikungunya infections in the Americas Dec 2013 to Nov 2014 (as of Nov 26th 2014) (Data provided by PAHO www.paho.org) |
Being a member of the Alphaviridae genus of the family Togaviridae, CHIKV has a positive strand ssRNA genome of 11.6 kb in size that encodes for both the structural and non-structural (nsP) proteins. In accordance with other prototype members of the Alphaviridae, the 5’ two thirds encodes for the four viral nsP (nsP 1-4) whereas the structural proteins are encoded within a subgenomic m 26S RNA, which in turn derives from a precursor 42S RNA. Both the non-structural (nsP) and structural proteins are expressed as polyproteins and cleaved by cellular and viral proteases. In the case of the polyprotein containing the structural proteins, following the (autocatalytic) cleavage of the Capsid protein, the remaining polyprotein translocates into the ER host proteases cleave the protein into the precursor E2 and E1 proteins both of which are N-glycosylated before being transported to TGN-46 positive structures -the viral replication center- in close proximity to the Golgi via NDP52 positive autophagy-like vesicles.
 |
| Prototype Alphavirus particle and genome |
 |
| CHIKV proteins and autophagy: NDP52 positive particles are transported to the viral RTC (model) |
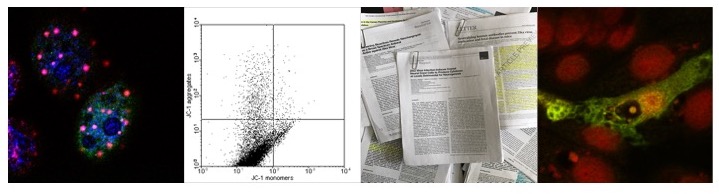
CHIKV and the ER stress response:
structural proteins
Since the polyprotein containing the structural proteins
(excluding the Capsid protein) translocates into the ER where it is modified,
expression of the CHIKV glycoproteins -namely E3E26KE1- by itself outside the
context of viral replication might be sufficient to induce the ER stress
response. Indeed, expression of the polyprotein in Vero cells results in the
upregulation of both ATF4 and BiP/GRP78 analogue to the expression of Sindbis
Virus (SINV) E2 and E1 proteins, as well as enhancing tunicamycin induced
expression of ATF4 and BiP/GRP78.
If however the expression of CHIKV E3E26KE1 under these
conditions also results in the induction of ATF6, IRE1, and subsequent
activation of Caspase -4/-12 as well as autophagy has not been determined, but
seems likely. It should be noted that in the case of SINV E2 and E1 proteins,
BiP associates with both E2 and E1 thus activating ATF6 and IRE1 mediated
pathways.
CHIKV and the ER stress response:
non-structural protein 2 (nsP2)
In Vero cells transfected with a plasmid expressing nsP2 and
treated with tunicamycin, at 16 h post transfection, tunicamycin mediated
induction of both BiP and ATF4 reporter genes are inhibited. Since this
inhibition is dependent on the ability of nsP2 to localise to the nucleus or to
induce shut-off of the host cells transcription by degradation of the catalytic
subunit of RNA Polymerase II, the expression of CHIKV nsP2 might inhibit the ER
stress response by inhibiting UPR associated increase in selective translation
induced by PERK phosphorylated eIF2α.
Since the expression of the viral envelope proteins induces
the ER stress response whilst the expression of the viral nsP2 protein inhibits
the same, the final aspect we have to discuss is if the infection of cells in
vitro and of mice in vivo with CHIKV induces the ER stress response. Following
the infection of Vero cells with CHIKV the induction of UPR reporter genes was
measured at 6 and 16 hrs p.i., at a timepoint where the induction of the ER
stress response induces autophagy as well as oxidative stress but when the
formation of the viral replication centers does not take place. Compared to
cells treated with tunicamycin (positive control), CHIKV infected Vero cells do
not upregulate the expression of GRP94, ATF4, or CHOP reporter genes despite
increased phosphorylation of eIF2α as early as 8 hrs p.i. . Taken together with
the results obtained from Vero cells transfected with nsP2 this indicates that
nsP2 is at least partly responsible for inhibiting eIF2α mediated increase of
reporter gene expression despite the expression of E2 and the E3E2 precursor.
Because SINV has been reported to induce the ATF6 and IRE-1
mediated ER stress response, it might be possible that CHIKV infection
mediates the accumulation of the spliced version of XBP1 and thus activates
CHOP. Indeed, CHIKV infection of Vero cells as well as primary murine splenic
macrophages and murine embryonic fibroblasts, partially activates XBP1 but to a
lesser extent than in cells treated with tunicamycin. Despite only partially
inhibition of XBP1 splicing, XBP1 protein cannot be detected in the nucleus of
infected cells, indicating that sXBP1 is rendered inactive. Additionally, spliced XBP1 is absent from tissue derived from
mice infected with CHIKV at 6 d p.i. despite displaying signs of CHKV specific
inflammation.
In the context of viral infected cells the inhibition of the
ER stress response by the expression of CHIKV proteins might be part of
counteracting an antiviral response induced by the expression of the envelope
proteins. The induction of the ER stress response not only induces autophagy
and apoptosis -both antiviral responses in themselves- but also triggers
inflammatory pathways, including p38/MAP Kinase, JNK kinase, and the NF-κB
mediated induction of TNF-α or IL-6. In
the case of CHIKV, this is corroborated by findings that both CHKIV nsP2 and
SINV nsP2 are potent inhibitors of STAT1 phosphorylation as mutations in CHIKV
nsP2 (P718S) and Sindbis virus (SINV) nsP2 (P726S) render replicons sensitive
to IFN induced signalling. The importance of nsP2 is also highlighted by the
observation that in CHIKV infected cells, nsP2 (in addition to nsP3 and nsP4) is stabilised by heat shock
protein 90 (Hsp90) and that inhibition of Hsp90 not only decreases viral
replication and inflammation but also nsP2 levels. Since in cells not expressing nsP2, nsP3, or nsP4 Hsp90 stabilises IRE-1 and is thus required for the induction of the UPR, it might be possible that the interaction with CHIKV nsP's contributes to the inhibition of IRE-1 mediated signalling pathways, including splicing of XBP1.
Further reading
Barry G, Fragkoudis R, Ferguson MC, Lulla A, Merits A, Kohl A, & Fazakerley JK (2010). Semliki forest virus-induced endoplasmic reticulum stress accelerates apoptotic death of mammalian cells. Journal of virology, 84 (14), 7369-77 PMID: 20427528
Rathore AP, Ng ML, & Vasudevan SG (2013). Differential unfolded protein response during Chikungunya and Sindbis virus infection: CHIKV nsP4 suppresses eIF2α phosphorylation. Virology journal, 10 PMID: 23356742
Mulvey M, & Brown DT (1995). Involvement of the molecular chaperone BiP in maturation of Sindbis virus envelope glycoproteins. Journal of virology, 69 (3), 1621-7 PMID: 7853497
Krejbich-Trotot P, Gay B, Li-Pat-Yuen G, Hoarau JJ, Jaffar-Bandjee MC, Briant L, Gasque P, & Denizot M (2011). Chikungunya triggers an autophagic process which promotes viral replication. Virology journal, 8 PMID: 21902836
Eng KE, Panas MD, Murphy D, Karlsson Hedestam GB, & McInerney GM (2012). Accumulation of autophagosomes in Semliki Forest virus-infected cells is dependent on expression of the viral glycoproteins. Journal of virology, 86 (10), 5674-85 PMID: 22438538
Akhrymuk I, Kulemzin SV, & Frolova EI (2012). Evasion of the innate immune response: the Old World alphavirus nsP2 protein induces rapid degradation of Rpb1, a catalytic subunit of RNA polymerase II. Journal of virology, 86 (13), 7180-91 PMID: 22514352
Frolov I, Akhrymuk M, Akhrymuk I, Atasheva S, & Frolova EI (2012). Early events in alphavirus replication determine the outcome of infection. Journal of virology, 86 (9), 5055-66 PMID: 22345447
Bertolotti A, Zhang Y, Hendershot LM, Harding HP, & Ron D (2000). Dynamic interaction of BiP and ER stress transducers in the unfolded-protein response. Nature cell biology, 2 (6), 326-32 PMID: 10854322
Rudd PA, Wilson J, Gardner J, Larcher T, Babarit C, Le TT, Anraku I, Kumagai Y, Loo YM, Gale M Jr, Akira S, Khromykh AA, & Suhrbier A (2012). Interferon response factors 3 and 7 protect against Chikungunya virus hemorrhagic fever and shock. Journal of virology, 86 (18), 9888-98 PMID: 22761364
Haze, K., Yoshida, H., Yanagi, H., Yura, T., & Mori, K. (1999). Mammalian Transcription Factor ATF6 Is Synthesized as a Transmembrane Protein and Activated by Proteolysis in Response to Endoplasmic Reticulum Stress Molecular Biology of the Cell, 10 (11), 3787-3799 DOI: 10.1091/mbc.10.11.3787
Lee AH, Iwakoshi NN, & Glimcher LH (2003). XBP-1 regulates a subset of endoplasmic reticulum resident chaperone genes in the unfolded protein response. Molecular and cellular biology, 23 (21), 7448-59 PMID: 14559994
Fros JJ, Liu WJ, Prow NA, Geertsema C, Ligtenberg M, Vanlandingham DL, Schnettler E, Vlak JM, Suhrbier A, Khromykh AA, & Pijlman GP (2010). Chikungunya virus nonstructural protein 2 inhibits type I/II interferon-stimulated JAK-STAT signaling. Journal of virology, 84 (20), 10877-87 PMID: 20686047
Smith JA (2014). A new paradigm: innate immune sensing of viruses via the unfolded protein response. Frontiers in microbiology, 5 PMID: 24904537
Fros JJ, Major LD, Scholte FE, Gardner J, van Hemert MJ, Suhrbier A, & Pijlman GP (2014). Chikungunya virus nsP2-mediated host shut-off disables the unfolded protein response. The Journal of general virology PMID: 25395592
Fros JJ, van der Maten E, Vlak JM, & Pijlman GP (2013). The C-terminal domain of chikungunya virus nsP2 independently governs viral RNA replication, cytopathicity, and inhibition of interferon signaling. Journal of virology, 87 (18), 10394-400 PMID: 23864632
Das I, Basantray I, Mamidi P, Nayak TK, B M P, Chattopadhyay S, & Chattopadhyay S (2014). Heat shock protein 90 positively regulates Chikungunya virus replication by stabilizing viral non-structural protein nsP2 during infection. PloS one, 9 (6) PMID: 24959709
Rathore AP, Haystead T, Das PK, Merits A, Ng ML, & Vasudevan SG (2014). Chikungunya virus nsP3 & nsP4 interacts with HSP-90 to promote virus replication: HSP-90 inhibitors reduce CHIKV infection and inflammation in vivo. Antiviral research, 103, 7-16 PMID: 24388965